I’ve had loads of information to process after my recent appointment with pain specialist, Dr Nick Christelis.
To prevent you all from zoning out (and my backside from having a fit), how about I spread my pain management report out a little?
If you’re in a kind of ‘I can’t be bothered, I’m over it’ and ‘don’t want to hear any recommendations or my brain will burst’ state then here’s a special post for you – Diagnosis: A Can of Worms.
And if you didn’t read how I prepared for my appointment please do so here because I’m about to reflect on it: Upcoming Appointment with my Pain Specialist
I’ll also be back to report on how I am going a few months down the track – sooner if something miraculous happens.
On arrival
It’s always great to see Dr Christelis and after my appointments I always feel very much relieved. There is such a huge psych component to having a specialist who understands you and your health issue.
If I just sat in Dr Christelis‘s room for half an hour I’d feel better. It’s the same feeling as when you’re with a great friend and you feel you don’t even need to speak.
Theo is always with me – he needs the appointment just as much as I do. Maybe for each patient appointment there should really be two made!
It was just minutes when I heard Dr Christelis say, ‘right, now let’s look at this list’. For a second I was really startled and couldn’t think what he meant. Then I realised he was referring to the list I made on my Pain Train profile.
Even though I founded Pain Train, I keep discovering unexpected benefits. I do log in and update significant information – the really important details that I don’t want to forget.
My history is so important to me and it’s also important that I record it in my own pain language.

That’s me up top with James from Boston Scientific being rewired!
Since the departure
I’ve had a few people ask me whether I will remove the peripheral stimulator and how the two devices impact. I’m not going to be hasty with any decision here.
I’ve seen a significant difference in pain relief and manageability between the sacral stim (Dec 2015) and the peripheral stimulator (Jan 2011)… imagine what might be invented years down the track? I’ve got to think about management, long-term.
Although it is tricky managing the two IPG’s in my backside, I’m better off getting to know the new stim a little more and making sure I won’t need the peripheral stimulator. I want to also make sure nothing changes with my situation – I’m in a huge life transition with the move away from Collingwood.
Obviously I want to keep my options open for an upgrade that may replace both stims. One that might be an even more advanced system.
I wouldn’t hesitate to remove the two stims if I knew an option for even better pain management was becoming available. I have so much faith in these devices and technology now. My brain responds to it.
Being positive and believing that one day this chronic issue will go or ease is my daily drive. But after all I’ve been through, I have also learned I should always have some kind of backup.
I feel I’ve managed to rewire my inaccurate pain signal by combining the stims and my ‘Can of Worms‘ attitude. Most importantly, the stims have helped me avoid medication intake/dependency – something that for me, was number 1 priority given my horrid response to meds.
Now, remember these posts are details from my experience and my pain management and relate to my personal chronic pain issue.
For you or for someone you know, all the details will be different.
I feel I can however confidently suggest that anyone with chronic pain leave no stone unturned nor disregard any little thing that might help.
It all makes a difference. It all impacts, it all contributes to brain change.
Sign up to Pain Train
I feel like I nailed the communication between myself and Dr Christelis. We were ready to go before I even walked in.
Fast, accurate, thorough, clear, smart, organised and independent are not the words I would have used in the past to describe me at a health appointment. This is how I would describe this appointment.
I still feel the relief today of walking in to the appointment and not having to worry about:
- where to begin
- what to say first
- what important advice I may forget to ask for.
The appointment was about ME – my symptoms, my specific problem. And Dr Christelis was able to answer my concerns – 100% accurate to my experience. He actually led the way.
I got the most out of my precious appointment. And I didn’t hear any general responses that didn’t related to my situation.
Feel free to view my (short, public) profile – specifically the ‘Patient Space’. Or, here is the list that Dr Christelis worked through with me before I had the chance to even pull up my profile:
Notes for Tuesday’s app with Dr Nick
- IPG giving me a few pains – not sure if this is due to weight loss (less padding!!)
- sensory issues with the sound of my hair, sticky tape dispenser and taring of paper when Theo is wrapping artwork a few meters away. Head moving on the pillow at night can be awkward as well.
- Still no daily routine established. It seems no routine is my best routine and I exercise in whatever way is suitable on the day. This could be 2 sun salutes, a 1km slow walk, a light 20 min yoga for pelvic pain routine, the hula hoop or walking on the spot for a few minutes – whatever I can get.
- Good heart rate lifter is plank pose but of course can’t always do it.
- Evenings are proving difficult. With my increased activity and attempt to work, I fatigue so normally I’d have little creative activities to do, a little drawing, or whatever. I’m finding I’m too tired but laying on the couch is painful – always has been. So Theo has to rub my feet, I put up with the pain, and/or I sit on the toilet alot… most comfy spot.
- Inflammation in fingers is becoming more often. Just coming out of a 5 week period where I couldn’t get my rings on and I’ve lost that kilo so very swollen and the joints are sore at night. Hips seem to be cranky too… perhaps the left side more.
- If I sit too long, my lower back and IPG area swell quite a bit.
- Overall though, much improved pain levels, have definitely paced up but limitations such as being in the car, shopping, lifting over the 3-5kg and the freedom to plan regular outings still rule the day
Dr Christelis offered the following comments/suggestions/recommendations:
- IPG checks out fine – I’m in the range of 5% of people who have IPG pain (and it’s not that bad just wanted to be sure).
- Research Hyperacusis.
- There’s nothing wrong with taking exercise when you can get it – routine not required.
- Stress about moving and changing life and beginning a new business was acknowledged as a really big deal and confirmed as something that would certainly impact pain and cause stress.
- Mindfulness, mindfulness, mindfulness
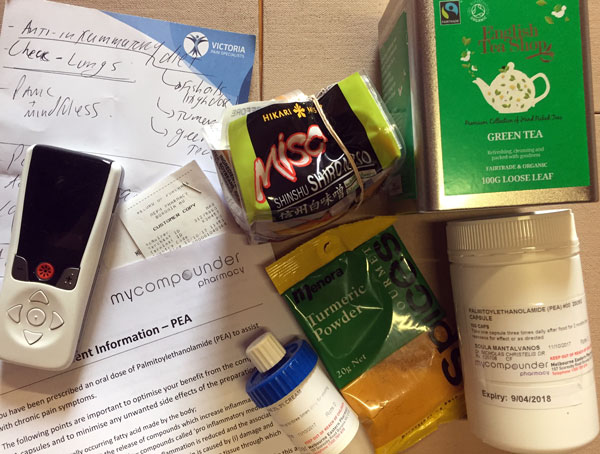
- Fingers and feet are within ok range but look into an anti inflammatory diet (include green tea, fish oils, miso, tumeric etc.
- My Compounder (THE best way to have medication prescribed and delivered to you!):
- PEA (we tried this prior to the stim and it made no impact) so worth trying again.
- A topical creme that cools and numbs.
- Check my lungs (can’t breath lately). Go to the GP and get some ventolin.
- Head upstairs, to James (Boston Scientific) and have the Burse program added to the stim*








Leave A Comment