I’ve had quite a few emails asking about my implant so I thought I’d create a more informative post. Given this device was a life changing treatment for me, I really haven’t given it its due attention. Implants are becoming more common for the treatment of pain, so it’s definitely worth getting my experience online.
I have to start with the pre implant status so you can all understand the impact the peripheral stimulation device had made for me (and I’ll call it my ‘stim’ if you don’t mind). I had just had diagnostic cortisone to my coccyx and had three wonderous days of complete relief. Hard to understand that’s even possible when a person can’t sit, stand, function without great levels of pain at every moment of the day.
I had presented to so many specialists (note the pages from my book, Art & Chronic Pain – A Self Portrait, of what my calendar looked like from 2007 -2009) and was labelled ‘the most severe case’ often. I had not been diagnosed as yet, I was lost, nowhere else to turn.
The complete relief response I had from the cortisone shot to the coccyx was ‘progress’. Has your practitioner told you in investigating your PN treatments that you might learn ‘what you don’t have or don’t need’? This is what’s meant by ‘diagnostic’. You almost have to work backwards with PN, cross off ‘what isn’t the case” and in my case, I had learnt I didn’t have ‘mechanical’ pain, I had neuropathic pain. My ‘mechanical’ surgeon, Mr Roy Carey, then handed me over to Professor Peter Teddy, and I have much admiration, respect and thanks to express for that moment.
I visited Professor Teddy (who is also a reputable brain surgeon), along with Theo who was lugging my kilos of scans with us and during the consult altered my sitting/standing/leaning position which was no relief mind you. Professor Teddy examined me, he suggested I leave my scans with him as he could present them to the surgical board he was part of. He also presented my case overseas to another board of surgeons as he happened to be traveling at the time. I felt hopeful knowing I’d be receiving many opinions from many experienced surgeons.
Professor Teddy returned from his travels (seemed like an eternity!) and had no explanation for my chronic pelvic pain. Most of his fellow board members had never even seen my white tail (sacrum/coccyx) and those that had could only say the white bone marrow presentation ‘was the difference between having blonde or brown hair’. I knew that made no sense, why didn’t my ‘colour hair’ extend to my spine and was only present in the injured area? But that’s another story and it’s called ‘bone edema/bone bruising’ but you’ll have to visit a rheumatologist to hear more about that. (Image of my white tail MRI as shown in my book, Art & Chronic Pain – A Self Portrait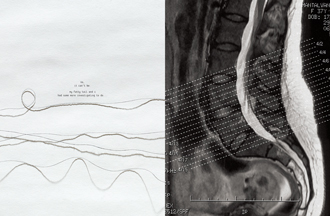 )
)
I begged Professor Teddy to do anything, even to chop my coccyx off but he (and his backed up opinions) suggested not to go the invasive path just yet (removal of the coccyx had also not been very successful in treating chronic pain), we had an option for an implant, a treatment that was reversible, it made more sense.
To ‘qualify’ for a stim you have to go through a trial first. The trial period was two weeks, I was admitted to hospital and the procedure was done under full anaesthetic. In that two weeks I had half of two leads placed inside my body, with the remaining half of the leads hanging outside my body connecting to a temporary unit. It’s a risky period, one very highly susceptible to infection but it allowed me to test the device and its impact before we implanted the $60k (or so) unit. Am I grateful I had private insurance? You bet! My WorkCover insurer certainly wasn’t going to pay, eventually dismissing the surgeons reports as not providing them with enough information to prove this was a relevant treatment.
At this point you might be thinking this sounds very similar to a TENS machine, it is. Except the leads of the stim are obviously placed even closer to the source of pain, and the closer to the pain source, the quicker you can disrupt/distract the signal to the brain. TENS did not work for me at all.
By the time my trial was done and I had an appointment where I could certify that I had 50-100% pain relief during this period which meant I could have a stim, Professor Teddy was planning another trip. I know you’ll understand me when I say it was like he told me I couldn’t have access to the only pain relief available to me, for a decade!! He was off in about 5 weeks, I remained hopeful and called his rooms every day in the event there was a cancellation before he left. There was a cancellation… I couldn’t believe it… I was in!
There was only one obstacle pre theatre: ‘Soula also wished to preserve intact a tattoo over her sacral region’, that’s actually stated on the report…! No, it wasn’t essential in the scheme of things but this was a tattoo of Botticelli’s The Birth of Venus and as Professor Teddy informed me while I was waiting to get into theatre, if we pierced Venus to place the leads, she may have ended up looking pregnant. There just wasn’t an option for a pure, newly born Goddess arriving on the shores of Cyprus to arrive in that state!
But back to the serious business at hand…the answers you’ve been waiting for:
Which model stim do I have?
I have a peripheral stimulation device model: St. Jude’s Eon Mini with two leads, each with eight points of stimulation, and the device which is in my left buttock (I have mainly right buttock pain). So that’s two small lead incisions plus the one larger incision for the unit. I have an external programmer (see below), recharging unit and a small magnet that travels with me to turn the programs on/off quickly. Peripheral means my stim is NOT implanted through my spinal canal but rather the leads are along the sacrum and coccyx (see x-ray image). Because my pain didn’t shoot up my back, my leads did not need to go through the spinal canal.
How effective was it/is it for you at reducing pain?
Incredibly effective for pain levels but the trick is not to increase your capacity beyond your limitations. The stimulation implant may or may not increase your capacity a great deal. The implant provided and continues to provide me pain relief so I can have a better quality of life. I was able to read again, concentrate more, listen and think for longer periods without the pain breaking my concentration. I could enjoy dinners/outings more (but I couldn’t increase the amount I went out by much)… well not until I was diagnosed about six months later. We all have to take into consideration our own effects of PN. Some might suggest I should have had nerve blocks before the implant but I have to agree with Professor Teddy and his response to me when I asked if there was any nerve he could block instead. He pointed out it was impossible to know where to start as I was in such a state. I now wonder if Professor Teddy had tried the nerve blocks first and I had not had a response due to the chronic state I was in, would I have ruled them out and not tried them again? That would have been a mistake. Rather, I look at my implant as having chiseled the glacier of pain leaving me with many smaller pieces that I was finally able to tackle, piece by small piece.
How long did this relief last? How you manage the device…
The relief is still effective today, three years on. The St.Jude’s team suggested I keep changing my programs. The stim is programmed for you/with you after it is implanted. Once I got used to using it and realised what I needed most, I called St. Jude’s and asked for more programs; a 20 min on/off cycle, a 30 sec rotation cycle, a one hour on/off cycle to help me fall asleep, etc and you keep changing this so that your brain doesn’t catch on to the programs. But as a pain specialist said to me at my recent presentation at AIM Pain 2014, ‘Soula the stim is a tango you dance with all your life and you have to keep changing your moves, keep with it and keep working with it’. I really like that explanation, it’s perfect. I thought I could try to eliminate the stim use with other treatments, concerned about the battery in my backside, but the better approach is to try to kill PN’s nagging signal as quick as possible and then eliminate the stim (if that’s even a possibility). So I’m piling all the treatments on now. I would call this another experimental phase.

The costs involved. What kind of stim do you have?
The trial was about AU$5,000 and the implant AU$55,000 but I had private health insurance and ended up out-of-pocket about AU$7,000 (plus Professor Teddy’s appointments). It’s not cheap and there are no guarantees and no way of telling who will get relief and who won’t, or who’s body is likely to react to a foreign object.
Is it true it’s no longer effective after two years?
As I mentioned above, you have to change your programs as our brains catch on, well that’s what’s worked for me. I’m still getting a great response from it.
And…
If you have more questions, please post them below so everyone has access to the information. Also, please note I am expressing my experience. PN and the stim are completely different experiences for each of us. This information cannot be used as a way to treat your PN issue.
To finish off, a great pain specialist emailed me this procedure link. Although it’s an interstim and a little different I will post it here as I can’t find a more pleasant clip to show the implant. It still basically covers the implant procedure.











Hi Kay. I imagine you may have found your way further through my website. You were reading a post from 2015. I’ve come a long way and had a sacral stim implanted since. Perhaps read here: https://pudendalnerve.com.au/2015/10/24/my-pain-management-is-turning-into-a-thesis/
The diagnosis or perhaps the understanding of what my issue actually is played a huge role. The realisation that I had to change my life to manage was key and we will all travel that path in our own way as we all have various tolerances, various priorities for the pain and so you have to make your own management plan.
This post: https://pudendalnerve.com.au/2016/06/12/who-am-i-going-to-be-soula-a-b-or-c/ might help you understand what I mean by ‘priorities’.
Also read here if you haven’t found it already: https://pudendalnerve.com.au/category/about-2/living-about-2/
Best wishes
Soula
Soula – Thanks so much for your post. It was encouraging to hear your story. An interstim was offered to me this week, so I’m just beginning to research it. You wrote that you couldn’t increase the amount of time by much you were able to go out, until you were diagnosed 6 months later. How did that diagnosis help you? And did that mean you had other treatments that helped you decrease your pain levels? I’m wondering what those were.
thanks, Kay
Hello Kimberley. There are definitely restrictions. Your specialist should be providing these details for you. You should have a very detailed plan about your recovery and what to expect after the operation. Recovery for the initial ‘stitches’ and implantation healing is tricky for about 5 weeks and upto 3 months I had to watch the twisting and certain sitting. The benefits far outweighed the recovery issues for me. Remember, we are all different.
I know this is an old post, but may I ask how recovery was? Was there restrictions on bending and lifting etc?
Hi Frances,
The ACCS and Workcover insurer found my implant was not acceptable treatment for my ‘psychological condition’. Apparently that’s what back pain is to them. I guess that’s what suits them.
I have never been able to sleep on my back since the accident but the few blissful seconds I have had (or when waking from a procedure after anasthetic), the unit has never been in the way. Only thing I’ve had to look out for is certain chair backs. I didn’t need to explore other options.
Good luck.
Hi Soula, I’m still waiting for work cover to approve my procedure. I was wondering about the placement of the battery on your backside. Is it annoying if you sleep on your back? Or when sitting? Did you have the option of abdominal placement? Thanks