It’s taken almost 9 years but I’ve realised that chronic pain requires alot of study – dare I say never-ending study? I believe my research for pain relief for chronic pain may be paving the way for a thesis!
I’ve had a good chat and stare with myself in the mirror, allowed the gut feeling to sink (for just a few seconds), called on gratitude, and here I present to you (with a backside that will soon be comparable in value to Jlo’s) another section of Soula’s Pain Management thesis.
Let’s call it Chapter 4 (approx.)
Patient: Soula (me) Age: 46 (& a few days) Chronic pain since: Mar/07 Injury: Drop to concrete floor from exploding fitball
SCS implant date: Nov 19/15 Procedure: Placement/anchoring of two 16pt Epidural leads inside the sacrum via the Sacral Hiatus & Neurostimulator/receiver Surgery time: Approx 2 hrs Device: Boston Scientific (Precision Spectra) Total Cost: Approx AUS$70k*
Thanks to: Medicare and my private health fund who covered more than 90% of the cost No thanks to: Victorian Workcover Authority & the Australian Workers Compensation system that refuse to acknowledge chronic pain and further stoop to certify this treatment as inappropriate for my workplace injury
Pain treatment history: Diagnosed at 4.5 years, 1 excision of thickened pelvic ligament, 3 x diagnostic cortisone injections (various parts of the pelvis and lower spine), piles of pain meds (tramedo, lovan, lyrica, gabapentin, etc), 3 nerve blocks, 1 x peripheral stimulation implant, herbs, various physical therapies (with various HPs) ie: physiotherapy, remedial massage, acupuncture, etc.
etc…
Review
The consultation began roughly like this with Dr Nick Christelis – Victoria Pain Specialists:
- I’m still very limited and rely so much on Theo’s help
- I was hoping to gain a little more capacity if it was possible
- I still have to avoid lifting anything above a couple of kilos
- Can’t lie on my back
- Can’t drive
- Car rides are restricted to about two a week
- Sitting with a cushion
- Sitting leaning on tables, arm chairs, forward all the time
- Can’t walk as far as I used to
- Everything is carefully planned for each minute of every day
And, I want to:
- Maximise capacity and prepare for an upcoming life change
- Work – current p/t design work is impossible
- Reduce the sitting demands – find a less excruciating way to make a living
- Sit without a seating aid
- Be able to manage short drives
- Manage as a passenger in longer drives
- Cook, clean, shop, etc
- Lift more than a couple of kilos…
…yadda yadda yadda
Method
Dr Nick Christelis helped me understand that my health issue requires life-long attention. Yes, I also heard ‘some nerve pain fizzles out’ and I will hope for that each day. But I can’t just sit and hope, I need to commit to the search for relief and treatment (no divorce options!).
Got it.
So I hopped back on the treatment trail and it wasn’t too many weeks before we came to the conclusion that it was worth me trialing another stim – Dr Christelis suggesting the leads be positioned inside my sacrum via the Sacral Hiatus. (Image below shows single lead inside Sacral Hiatus)
It made alot of sense to me – why wouldn’t you put the leads as close to the source of pain as possible?
The trial
Duration: Two weeks 24/7 SCS trial date: Sep 08/15 Procedure: Placement of two 16pt Epidural leads from inside the sacrum via the Sacral Hiatus to external Neurostimulator/receiver Capacity level: Increased immensely Pain level: Reduced immensely Result: More than 50% relief, therefore successful
Trial Details

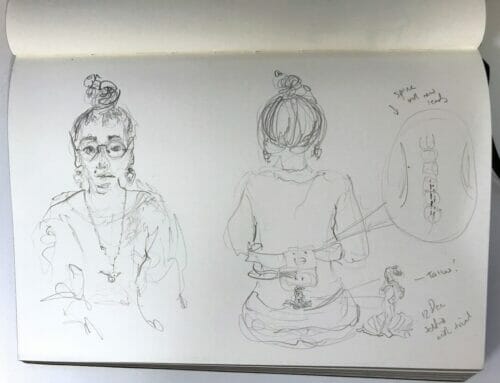
Xray showing the sacral stim trial leads with 16 points in each lead positioned inside the sacrum and the external receiver at top. Also visible is my peripheral stim with two leads identifiable by their 8 points each and the implanted receiver.
Yes, a trial is difficult. The biggest issue being the risk of infection as the leads literally stuck out of my back and were taped to the skin.
I had post op pain, I couldn’t shower, I had a belt and receiver strapped to my waist 24/7 but in the scheme of things, for me, it was not an issue. I lapped up the increased capacity and low pain levels. I was off!
I find post op pain much easier to handle. It doesn’t rise to take over your brain and fatigue you. And just knowing it will go makes the difference.
With Theo in the driver’s seat, at the 7 day mark we traveled from home to my favorite gallery Heide MOMA, then to Dr Christelis for a checkup, and on to Castlemaine for a weekend. Google tells me we travelled 275km one way!
I held a handbag the whole weekend, didn’t have a seating aid (except during travel), went out for breki, lunch and dinner, enjoyed the ride in the car to surrounding towns (I was able to sing in the car which usually hurts), and even got back home in wonderful form to allow us to head out for the evening! Unheard of for me.
The end of the trial is marked by all of a few minutes of removing bandages and about a second that it took to slip the leads out of my body.
I know, wild!
Not so wild was the wait for my real deal implant. A whole 8 weeks!!! But I had residual lasting pain relief confirming my thoughts that this nerve monster is truly a cruel beast but an implant was the right idea.
Brain, can’t you just hold that pain-free thought- you know the one you’ve known most of my life?
(Get on with it Soula)
The implant
It was a great long nap… two hours approx. It’s such a treat to wake on my back and to sleep and sleep without pain interrupting. I did that, two decent days worth of just napping. Deep sleeps. Bliss!
I’ve written about Vicpain‘s approach in previous posts. I’ve only once experienced this level of care and patient/practitioner equality – the feeling that someone is paying attention to my situation and treating ME – a person.
It was extra support to know that Vicpain‘s Dr Christelis, Dr Simon Cohen and Dr Tim Hucker work as a team. To put it in patient terms, these guys hang out together alot, even in theatre, learning, helping out with each other’s cases. That’s impressive.
From my very first appointment, to my prep for the trial and implant, to the very last blink before that sweet anaesthetic, and throughout my post op care, I heard a consistent manner and tone from Dr Christelis.
For both procedures, I saw Dr Christelis before theatre – in fact he sat with Theo and I and we went through the patient consent form together both times. Responsible much? Totally!
I knew exactly what Dr Christelis planned to do and planned to avoid, I heard the risks, and then I heard the plan again. Same warm tone, same open conversation… and there are handshakes and smiles galore. And Theo was kept in the loop at all times.
Why haven’t l always felt this cared for, dare I say – important? And why am I harping on about this approach? Because I believe it makes a huge difference.
Feeling aligned with my health care practitioner places me at the forefront, it feels more honest where previously I felt pushed back a couple of steps. Health carers can often leave you feeling awkward, like you’re too needy and there’s some secret society behind theatre doors.
I’ve felt out-of-place and kind of like I rocked up at a party uninvited. But isn’t the party for people in pain? So it only makes sense that both the practitioner and patient attend. And you better both have your dancing shoes on!
One guess what this approach did for me? One guess what it did for my confidence? One guess what happened when I came out of this new treatment? I felt as armed to handle my health condition as I most possibly could. And I learned I was most responsible for it.
I kept hearing I was responsible, and I’m still hearing that.
And now, after having moved to a more suitable location and overcoming the idea that we were settled in Collingwood, after having completely changed our lifestyle and planned a new way to make a living within my limitations, after finding a dedicated and caring pain team who have provided me with the most suitable treatment (for now) – I can wholeheartedly say that Theo and I have committed and are as responsible for my chronic health issue as we can be.
A patient with chronic pain cannot do more than that.
“The absolute key is to have a motivated, proactive patient that understands the technology and the limitations too.” Dr Christelis:
I’m guessing there may be questions…
Does the implant work?
What I mostly feel now, is post op pain. Stitches pulling, tugging, aches, stabs and oh those itches! All of this, I find easy to manage with basic pain killers. The neuropathic pain is dramatically reduced and I’ve been much more active than I was before the implant (my post op limits offer much more activity and ability in comparison).
What would I be worried about?
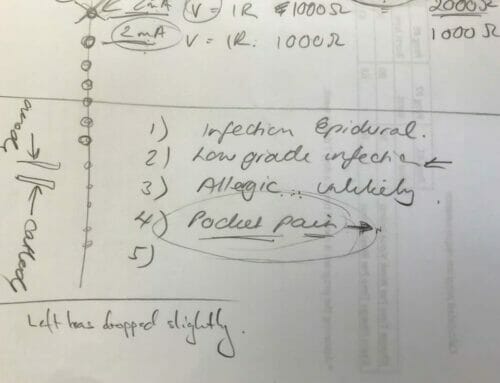
As Dr Christelis put it: LIPS
Lead migration
Infection – superficial or deep.
POCKET pain – pain at IPG (implantable pain generator)
Stops working – looses effects over time.…
Yes, I also nearly threw up at the last point but don’t all pain treatments lose effect? Aren’t they all just a form of distraction? I believe Lorimer Moseley covered that one with his latest post, Explainer: what is pain and what is happening when we feel it?
I’d like to think my previous peripheral distraction hadn’t lost its effect over time but rather I increased my capacity. Also four years in medical research is a huge amount of time when it comes to pain management treatment. Obviously a newer implant is going to be more effective – I want more capacity and less pain. That’s what Dr Christelis wanted for me too. He found the way and I believe he will keep searching for a better way.
So far – no worries. I’m feeling spectacular.
Where is everything placed?


(Right top: Placement of new stim top left buttock cheek with a glimpse of the peripheral device below. Right bottom: sacrum with both leads in view (old and new and a glimpse of the wires down below)
Aim
To remove the peripheral stim within 6-12months.
Can I feel the stimulation?
Yes, sometimes but not always. It’s going to take a while for us to get to know each other. It’s all new again. Don’t forget I have an extra 16 points of stimulation and each point is individually programmable.
So that means from my sacrum down to my toes, I’m programmable. Thumpy, fine, wide, spread out, strong, subtle, twangy, tingly, or silent pulses… I can have them and in any or every spot I need. Perhaps stronger in one place and lighter in another, or off in one spot and full-on in another? It’s all an option and all options are at my finger tips.
Programming info
Once programmed I have a kind of phone gadget I use to control my stimulation. I’m programmed like this:

Recharge?
Yes, recharged depends on use. But I need to recharge my controller and my receiver. Not even worth showing really.
Invasive?
Sure, a bit but in my opinion much less invasive than surgery to the Pudendal Nerve or removing any bones.
Summary
I could have made this post alot longer but truth be told, I want to get off this damn computer. I’ve got things to do. I am ready to begin a new life.
I’ll only say that finding treatment for chronic pain is really hard work and takes commitment and research enough to make a thesis or two! There’s no short cut, in fact the long, slow road is the shortest way possible.
In the two weeks since having this treatment I’ve been pottering around, building our new venture and preparing for our new life launch. I have a sense of peace and comfort knowing that with Vicpain‘s help, there’s been no stone left unturned in our quest to find quality of life and the best form of pain management.
We’ve done our best. Chapter 4 (approx.) is complete.








[…] be honest, I’ve been a bit over it the past few months with my Sacral Stim playing up – or is it my […]
Dear Soula – its been some time since I wrote so here goes – I have been the impossible client to my doctors, who seem to know little of prudential nerve pain. So I have kept my eye on you and your search which helped a lot. Just to know someone else was on a very necessary answer. I centred on cryoablation but VicPain said NO. They advised on neurostimulation and said surely NSW can do, if not come down – I live in Forbes centre of NSW – so I am lined up with Sydney North Shore Pain Management – it s considered the best. It could be a long wait or they may not accept me. I live on Lyrica and Palexia with panadine forte for flares, it works sorta. I am so pleased you seemed to found some relief. I just finished a Pain Management e course with Macquarie University of NSW it is really worth doing. While I have not been obvious, nevertheless I have daily followed your life, a few knots in the string but now on firm ground – Good on Ya.
Yarra at Forbes NSW
Forgive my late reply Yarra. I hope you find some relief. Please don’t stop believing things can change. I still remember the first second the pain wasn’t there… that second became two and then three. I know it’s slow but I do believe now that the brain does change the way it harps on about pain very slowly.
I can’t recommend Vicpain highly enough but not having to travel certainly makes a big difference.
Thank you for the encouragement.
On ya too!
Soula, I want to subscribe, but I don’t use PayPal.
Is there any other way I can subscribe, please?
I admire your handling of your chronic pain, your attitude towards pain and your blog posts.
I, too, am on my own pain journey, I have SCS implanted but depend heavily on my self-management methods as the underlying disease progresses and medication simply doesn’t help.
I look forward to following you on your journey, and to adapting your methods and ideas to my own situation. Online help is essential for me, as I live in NW Ireland, and have long journeys to travel to consult with my medical team.
Many thanks,
Frances
Dear Frances,
I have added new information on the subscription pages. You can pay by credit card on the PayPal website without saving your information or creating an account.
You can read more about that here: https://www.paypal.com/webapps/mpp/account-optional
Or if you feel more comfortable, I can email you direct debit details.
We have quite a battle and we can only do our best. I hope your SCS is helping and that your strength continues. It is so difficult living far away from treatment… but here’s hoping you find a way and the appointments lessen and quality of life increases.
Thank you so much for leaving a comment and for subscribing.
Hi Soula
I am delighted to receive this good news.
In my opinion, the Victorian WorkCover system has a lot to answer for by failing to support you when you really needed help.
But all that nonsense is now behind you and no one can say that you did not try your hardest to remain a productive person in the work-force.
Happy New Year to both you and Theo.
Love from me and Cynthia
John Quinter
I am so happy to hear this, Soula! And I do hope that you will share your new adventures with us but also know that it’s ok if you don’t – just go out and live for a bit and only write if you want to :) This warms my heart so much today, I can “hear” the excitement and hope in your words and I couldn’t be happier for this new part of the path in your life. You are absolutely right that having a healthcare professional who listens, is empathetic, who is knowledgeable and giving of their time, words, and care is so important. We need to feel validated, believed, and believed before we can ever start moving forward, before we can have the confidence to be responsible for our pain treatment and management, I think that is too often overlooked. Yes, we are responsible, but we have to know what we are responsible for, we have to have understanding and be understood. We have to be heard.
Sending you love and hugs and pain-free vibes, my friend! xoxo
It was supposed to be validated, believed, and trusted – not believed and believed but that’s pretty accurate, too!
I actually thought it read perfectly. Your support is huge to me. Thank you, you get it. Huge love and hugs right back to you dear friend xxx
I applaud both you and Dr Christelis on your commitment to problem solving and sourcing pain relief options and sharing these facts. I am so happy for you that your pain has been reduced and an increase in capacity ensued. What model stimulator did you decide to utilise? All the best Soula in your new adventure.
Hi Kathryn, I hope you’ve been well. It is problem solving, neverending problem solving. Thank you for your wishes. Details of the stim at the top of the post. It’s a link to the official page.