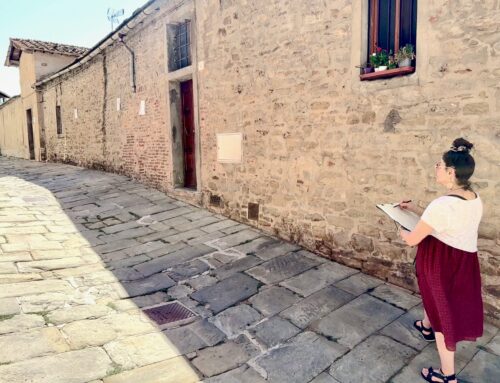
(Image: Pendulant, acrylic & graphite on linen. Wonderment exhibition at Queenscliff Gallery & Workshop)
That was my endnote for 2019.
As life evolves within my 3km radius, I find myself looking back less and less and looking forward more and more.
Bitter, defines the heartache of not being able to see loved ones as often and the missing perks of our previous city life.
Sweet, is being defined by new friends, the gallery, our new home and the sea that surrounds us.
As for confused, another year has passed and I still don’t feel anyone can quite define what’s going on with my body.
Does it matter heading into a new year?
Confusing Definitions
First allow me to specify – I’m talking about ongoing, chronic neuropathic pain.
Chronic pain is defined as pain that continues past 6 months. What I’m referring to (and always have referred to) is pain that continues far further than that… further into years.
I believe there are two steps there, not one. I believe there is a difference but I can’t prove it.
Another thing I believe – that I can’t prove but am not confused about, is that we all experience pain differently.
There are layers. There is a variation of intensity within those layers, a variation in the ability within the layers, and there’s the question of whether the pain will go, stay and in what capacity it will go and/or stay – it’s a unique scenario to each of us.
No one can formulate a fix for all situations. No one should say they can.
I don’t think anyone can prove they hold the definition of pain. No one should say they are certain of anything when it comes to chronic neuropathic pain.
We’re all just hovering in a moment in time. We’re here with a load of ‘findings’.
What I know for certain
My experience shows me two things help me manage pain:
- Adapting my day-to-day life
- Neuromodulation
That’s been certified for me! And this does not confuse me.
I think of the pain world as a pie that is made up of:
- Consumers – people living with pain
- Managers – pain professionals and scientists
- Followers – pain organisations/government
People are being presented stats and data and everything we ‘learn’ and every treatment explored seems to be another trial.
As humans and sciences evolve the advice will continue to change. And then change again.
We can’t know for certain that what we hear right now is correct or incorrect.
The Followers are just preaching what they hear. They offer nothing.
People in pain are really all alone. Alone with pain.
Diagnosis
The diagnosis is chronic neuropathic pain.
That’s what my experience was titled and that title suits any experience of long-term neuropathic pain I believe.
I’ve learned not to demand more or less of this title.
Any other definitions surfacing have not been able to provide clues to further my pain management or to help solve my problem.
I find the nitty-gritty of science and various beliefs offered to a patient are kind of thoughts in the air… more ideas to try.
My personal developments and failures didn’t stem from what I read or learned, they stemmed from my experience and through the moments I spent with pain.
I didn’t meet spasm on a page, I met it through flinches on my skin and strange toilet functions.
I didn’t burn my fingertips reading about a flare, I felt it on the inside of my pelvis.
And I certainly didn’t gather my initial understanding reading pain research or after I visited my GP or pain specialist. I had experienced this pain for 4.5 years before I was delivered the title.
I look back now and can see that all I heard and read about living with pain, I knew already. And today, all I hear and read about living with pain I know already.
I remain confused by the information about this experience that’s on offer because it usually identifies characteristics of my experience without giving me a solution.
2020
In 2014, Dr John Quintner contacted me to wish me luck before my first-ever presentation (at the Alliance for Improving the Management of Pain).
I’ll never forget his words as he was trying to encourage me – I was so nervous. What did I know in comparison to the 200 pain-interested professionals that were attending this conference? What could I possibly have to tell them?
‘Remember, you will know more about pain than anyone sitting in that room’
My physical, day-to-day living – that is each second in time with this experience, is what guides me to the next.
I may be guided to another flare or to an hour of pristine pain-free time but that is the truest fact of what pain is.
In my new life, I believe I have gathered the best treatment possible and see the best specialist. I’ve always had the greatest possible attitude to management throwing myself into as much research as possible. And my complex health files are in super order.
With or without my confusion, I know what I’m doing each day now – I just don’t have any meaning for the experience or the solution to the problem.
I’m getting used to being in my state of pain confusion. I am recognising it as the way of my life. So do I need to keep reading and searching?
I might just stay right here, in: ‘I don’t have the definition of pain but I’m establishing a way to live with the experience’ and rather than lose more time searching for meaning, spend time progressing my new life further.
To be honest, even if the world’s greatest health scientist, the Great Oz, Darth Vader or a talking dog were to deliver a definition of pain to me right now, I don’t know I’d be able to believe them.
I’ll believe a definition when I experience the solution.
Until then, I’m going to sit with my confusion, my bittersweet new life and with what I’ve learned from my experience because it’s as real as I’m going to get. And it’s as proven as it’s going to get.
It has provided me with the best direction so far and the most information I can bank on for my future.
I’m going to pull the plug on the big questions this year.
I’m going to try and just be during 2020.
Yours,
Truly confused,
Soula










Wonderful comment Jay, thank you!
I still think Tame the Beast, Dims and Sims, and all Lorimer’s work is valuable but as we both agree, not all explanations fit everyone’s pain and I think that’s the most confusing bit. We stream our posts and jump into them without getting full context.
Mechanical and nerve pain is the way I categorise pain. And when describing it I often refer to chronic fatigue. A tiring of the system that can even make waking exhausting.
You’ve given me some more very valuable info. How interesting (and what a relief) the approach to phantom limb pain is.
I hope there is more help for us. I just might take a break from tuning into the nitty-gritty so wake me if you find something won’t you? ????
Thank you again for leaving this brilliant comment.
Take care.
Thank you my darling. Always sad to read that followers relate and how they relate – we share that frustration especially at this time of the year. Yes, I’m sure we’ll be fine and happy but you are so right in saying it won’t be our best self. x
That gets me thinking about sleep and pain. And anaesthesia and pain. It certainly implies that someone living with pain has less control. That is easier to swallow but obviously I’m still left without a solution.
Every person is an individual. There experience with pain unique. There is no defining how to treat neuropathic pain. There are different modalities that can help. I have been helped by many caring medical professionals . The patient knows their body best and in my experience when the medical team listens to the patient and doesn’t assume, the patient gets the help they need. If one modality does not work move on and find another and maybe even return to the first one. Chronic pain can be managed but Pudendal Neuralgia specifically is quite devastating. To focus on the devastation makes it worse. So, I give my self a daily pep talk and get my butt out of bed in the morning and accept my diagnosis. I accept I have to awkwardly excuse myself socially when my nerve decides to take over my bowels. I have told my coworkers I have sought cognitive therapy for my problems and it is what it is . I have to accept it. To try to hide this diagnosis is worse than the diagnosis. People can accept hearing the words Chrohn’s Disease, Fibromyalgia. Multiple Sclerosis, but Pudendal Neuralgia???? Are you kidding me. What the heck is that????? Maybe I will be the first one to say it out loud for people to hear it publicly. Maybe a commercial on tv about it will help bring awareness. This could help the patient more than medication. What is neuropathic pain???Hmmm, put your finger in an electric outlet and maybe then define it.
All kidding aside it helps to vent frustration and form a community of people to help each other. If we don’t laugh then we will suffer more from isolation. I recently had a coworker make sport of me when I was absent. It hurt so deeply that someone would take my misfortune and ruin my reputation. I had to suck it up and move on.
Hold my head high and say this is not my fault I have this problem. No one wants to be around people with bowel issues but oh well too bad that’s life. I am a person and I have worth. You can be around me if you want to if not your loss. I cannot change my diagnosis .
I continue to improve myself in every way I can. I will be part of the world in which I live. I want people to hear this. We all have value.
Great article Soula. It’s hard to make meaning out of long term pain. I read Vicktor Frankl’s Search for Meaning book last year. That helped me.
Yes, I think people who have their brain stuck in a loop have Complex Regional Pain Syndrome?
Personally I know I don’t have that because my neuropathic pain has been constant & predictable ever since my back injury, eg I know pressing my right foot down to drive is excruciating & causes my sciatic nerve pain to flare up, but taking weight off my right leg & butt helps settle the nerve back down.
I don’t believe it’s possible to conquer nerve pain with your brain. That’s the line insurers promote, because they don’t want to pay people for injury & permanent disability.
I noticed my insurer EML sponsored the research done by your pain “scientist” friend Professor Moseley. I think he may be contributing to your confusion. I listened to one of his talks & watched his pain video Tame the Beast, but I disagree with his findings. He uses the fact that some people feel pain when there may be no reason for it, as a way to dismiss people’s legitimate pain.
One of his examples is phantom limb pain. He says there’s no reason for it, because the limb is no longer there. But research is showing that phantom limb pain is caused from the severed nerves, that are still reacting with pain or other sensations. The nerve pain is not protecting the body, which is the only function he claims as being the reason for pain, nor is it pointless. The nerves are communicating to the body that something is wrong. There is an issue with that nerve & that limb, it’s been amputated!!
Because of phantom limb pain they have now learned when removing a limb to not sever the nerve but to leave as much of the nerve intact as possible. This aids in healing & has reduced the incidence of phantom limb & neuropathic pain for amputees.
The nervous system is like a closed circuit electrical system that runs through the body & they are realising that when there is a break in that system it stops the electrical impulses from being able to travel through the body as normal. This disruption to the flow causes pain signals to alert the brain that something is wrong & that the electrical signals can’t travel as normal.
Prof Moseley’s other example of why pain isn’t real because it can get worse when you feel stressed, anxious or angry…was explained to me in my first session with my pain specialist, as being because pain is processed in the limbic system, which is the same part of the brain where emotions are also processed. This means that pain triggers emotions such as sadness, anger etc, but emotions can also trigger pain. We know the nervous system connects straight to the brain, so of course neuropathic pain is going to affect our thoughts & feelings in the brain. As part of managing my pain, I have to manage my emotions, as stress or anger does havoc to my nerve pain.
I think prof Moseley is correct when he says pain acts as a protective mechanism, but that is in normal instances of pain, for responding to external stimuli outside the body. But when it comes to neuropathic pain, it’s an internal issue, and more of an alarm system to alert the body that there is a problem. It can feel like my alarm is permanently stuck on…but in fact it isn’t. It still warns me if I’m stretching the nerve and making it worse. I don’t know how it is for you??
The central nervous system is really complex & there is so much they still don’t know. I hope they find more help for us in the future!
Thank you Soula for your honesty.
As we enter another year, I find myself reflecting on everything that I have lost, and find it very difficult to think of what I have gained.
I look at my children, men now, aged 29 and 31. They were 4 and 6 when I was injured. Do they remember their Mummy laughing, running after them on the beach, riding bikes together in the forest? I doubt it…
But I remember; I grieve for those stolen moments.
Today is Mark’s last day off before he returns to work to provide for us. We are trying to get out and enjoy the crisp, Winter sunshine. I am sitting on the bed psyching myself up for a car drive, and the impending loneliness that will descend when he is gone for more than 12 hours a day.
I miss living.
This year I am determined to find a way to embrace “what is” and “who I am now”, instead of wishing for the past.
Sending you and Theo much love and all best wishes for this coming year. May we both find and cherish those blissful, brief moments where we are “painfree”.
Thank you again for this beautifully written article.
With love,
Sue xx
Soula, we will experience pain whenever activation of our nociceptive apparatus reaches the level of consciousness.
Soula I am truly sorry that pain is still part of your life nobody should live with daily pain and for such a long time pain stop us from being our best us and putting on the happy face can be hard when we are having a bad day I am over repeating myself to health professionals and educating them on Pudendal Neuralgia explaining to family why I can’t go to event but you Soula will move into this year will your wonderful husband by your side with all your talent and many people around you that love and respect and admire you as a courageous can do gal lots of good times are also ahead for you Debs
So frustrating isn’t it?!
And no one can argue with you Joan. Nor me! I’ve heard my specialist answer honestly several times, ‘we don’t know’.
Could there be various explanations John? Could there be instances where the pain is in some loop and in others where the reason is different? Why does there have to be one explanation? Oh dear, I asked more questions….!!!!
I do feel the pressure of having to control my brain and that is so difficult when others are staring at you stating they conquered theirs!
Thank you
Soula, pain cannot be imprisoned within a definition that will satisfy everyone.
Well-meaning clinicians are attempting to explain pain as if the experience is solely based on a decision made by the person’s brain.
Evidently our brains can make wrong decisions when pain is experienced and there is no evidence that the person’s body is in danger.
Of course this dictum is folksy nonsense.
Moreover, it exposes the person experiencing pain to an increased risk of being stigmatised.
This is not a desirable outcome!
I have lived with unrelenting pelvic pain for 16 years now .I have been told many times that the medical profession know very little about neuropathic pain and that is certainly my experience.
I could have written this myself Soula.