(Photo credit: RACGP Victoria)
I’ll deem my efforts a success.
I managed. I learned a bundle. I made something of the chronic pain experience. And I believe I provided some insight.
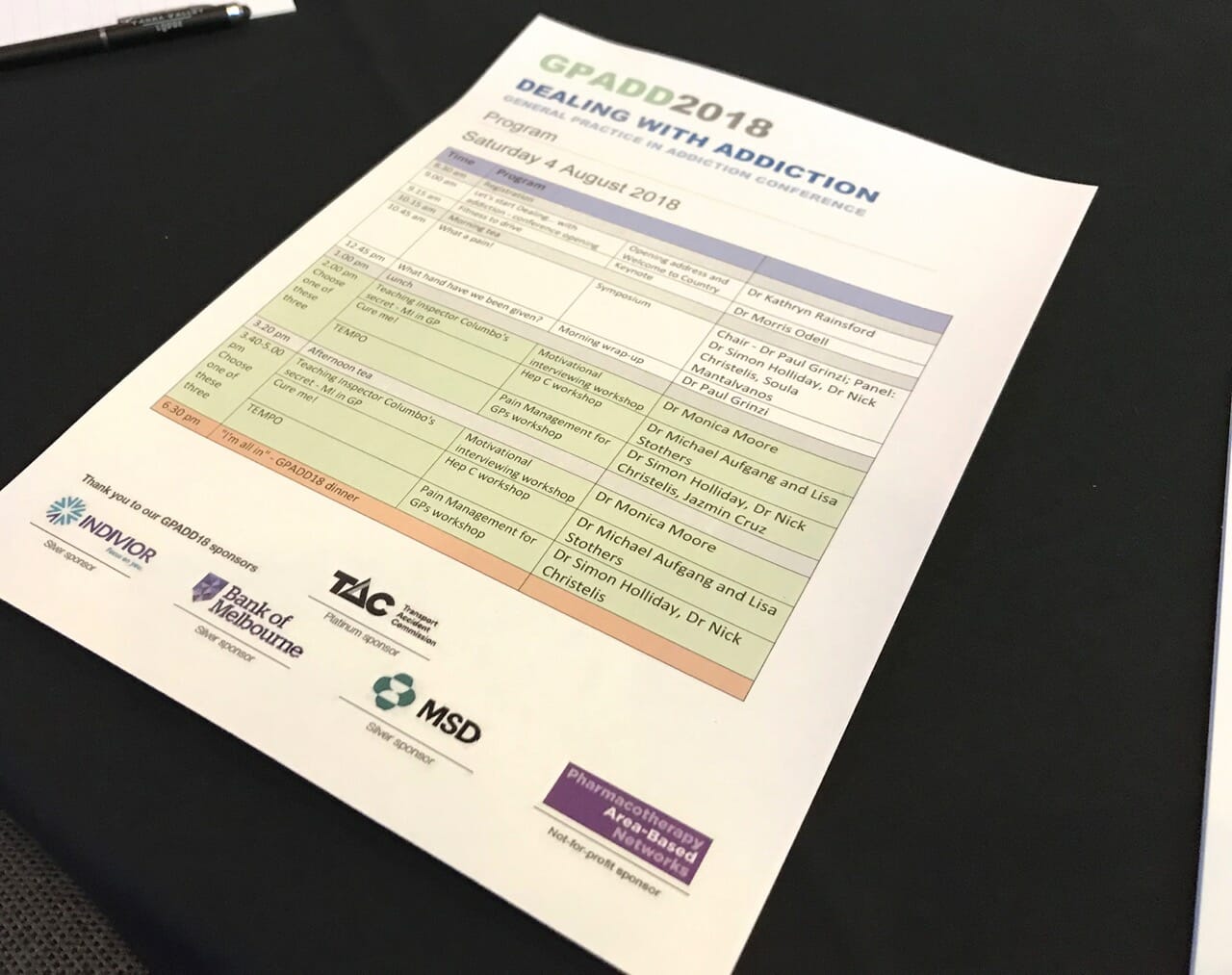
I arrived at Yarra Valley Lodge on Thursday night and left Sunday early morning to manage the presentation, question time and a short attendance at the dinner on Saturday evening.
So that’s 3 night’s sleep (and one nap Saturday afternoon) to get the focus I needed, and so I could appear in a way that I felt reflected my most Soula self. The presentation (below) took weeeeeeeeks to put together! Something that would have taken me a few short days previously.
That might sound alot of sacrifice to many of you but with this approach, my pain levels remained low (if not off) and on my return to Queenscliff, I could resume my part time work and the week ahead as per normal. It worked, I’m pacing up!
I do have a niggle though. We’re not learning fast enough. We’re not listening hard enough. I left disappointed I hadn’t achieved enough.
The good stuff
I mean how amazing is it that a patient was invited to share their story and resources?! Without the consumer feedback, no product or service can survive.
And the GP’s who attended, together with the organisers obviously know this. I’m going to call it a glitch that my resources didn’t make it to the attendees or perhaps my lacking professional qualifications got in the way. Liability ruins so much opportunity.
The resources I shared are ones you’ve all seen over the last few years on this website except I collated them all in one live linking pdf. They are included below.
The daunting stuff
It feels to me that the real battle for both people in pain and professionals has more to do with behaviour change.
I’ve been bringing this up in recent posts as changing behaviour is a huge part of my professional work – a designer produces a creative solution in hope of inspiring and motivating action and that action is generally a call to embrace something new.
I presented during the What a Pain Symposium. I was third in line after Dr Simon Holliday (amazing!) and Dr Nick Christelis (pain Einstein and my specialist) and then a Q&A followed.
During that time one question I was asked was, ‘what could a GP say to a patient in order to help them manage their pain experience?’.
These incredible caring humans are concerned, they are compassionate and want to help. But my answer wouldn’t have been too helpful. I had been thinking about that question and expecting it but all I could come up with was;
to help a person (living with chronic pain) understand what they are dealing with, you need to somehow get them to switch to a new belief ethos – same goes for the professional!
Eg If you believe in God, now try and convince the person God actually isn’t there or vice versa. Another example might be if your cultural background is Chinese, now try and direct the person to live like a Greek person… almost impossible!
But, that approach is what is required to manage and understand pain.
I can’t help but think that everything we have been taught about pain, in general, seems to have no relevance to chronic pain.
There’s a template learning for GP’s and that includes about ONE FULL hour of chronic pain education. There’s a ‘model’ of learning and the current research for chronic pain doesn’t fit with that model. It’s new.
So go on then. Try it! Go up to someone who believes in one thing (and has done so for all their life) and try and get them to comprehend that the ‘facts’ as they knew them have changed… and it just happened in the past few years.
Actually, most of you have been trying to do this, I’m sure!
Where to?
I wish I could be put in charge of the media for chronic pain for Australia. Manage the branding of it and police the stupid ads that keep portraying examples of people who don’t have time to be in pain, or portray the heroic some who can simply pop their pills and keep on lifting!
Remember ‘Life be in it’ ads? Where did they go? Norm was so clear about health management…
It’s going to be slow, really slow and that means really complex for those living with pain. The waiting periods to see a pain specialist (because it’s confirmed this IS who you need to see to mange pain) are 2 – 3 months in either a private or public system.
I do see the interaction from my posts and it’s a general rule that my posts encouraging people to educate, sacrifice, and/or change their ways are less popular than the ones where I talk about my day to day response.
Our general behaviour (stemming from the silly ad messages during our lifetimes) of going to the GP and expecting a solution is holding fort and that sadly isn’t going to get anyone near lower pain levels.
It takes sacrifice, commitment – a person need’s to put their life on hold just as they would if they were diagnosed with cancer, heart disease, etc. Chronic pain needs your attention – full attention or it will keep screaming through you.
My presentation
I wasn’t able to film during the conference for obvious reasons but I have put together the graphic presentation with my voice over.
WARNING: This presentation contains calls for a new approach to the management of chronic pain. It calls for bundles of learning for both professional and patient as well as sacrifice and 100% commitment. It’s a little boring and most disheartening for those on the search for a quick fix.
In this presentation:
- 0:28 Outline
- 0:43 About Soula
- 0:58 The accident
- 1:44 Chronic pain treatment & investigations
- 2:19 The peripheral stimulation implant
- 2:36 Diagnosis
- 3:00 Quality of life
- More treatment
- 3:27 Communicating Pain
- 3:50 What is our understanding of Pain?
- 4:50 Resources for pain
- pudendalnerve.com.au
- The Hurting Strings Documentary
- My book Art & Chronic Pain
- 7:14 Changing our ways
- New definitions
- 7:48 John Quintner
- the third space
- pain is like love
- 9:21 Explain Pain
- Prof Lorimer Moseley / David Butler
- What should we know about pain?
- 10:40 Changing our behaviour
- Protectometer
- PainTrain – My Health Summary
- 11:20 Example management
(how I managed the talk) - 11:28 PainTrain examples
- first appointment healthcare scenario
- postoperative healthcare scenario
- follow up specialist appointment scenario
- 15:28 Conquering pain management
























Leave A Comment