It’s time we talk about the addiction killing more Australians than heroin and ice combined.
(Excerpt from mamamia.com.au. Story by Caitlin Bishop)
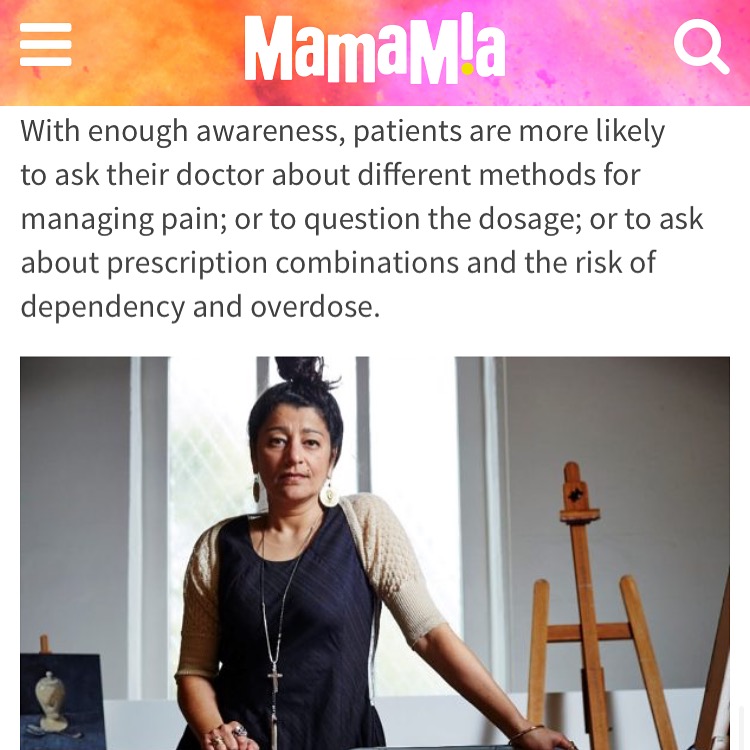
Soula Mantalvanos was 37 when she was sitting on a fit ball and it burst. She landed on concrete, hard.
“It was a split second. It was bone to concrete and it felt that way. I was in shock and then thought ‘I can’t move, I can’t move’. Slowly, I turned over and crawled to the carpet,” Soula told Mamamia.
Before then, Soula walked everywhere. She lived with her partner in the heart of Collingwood, Melbourne. They would walk to see friends, walk to dinner. Soula did yoga four times a week. She could hold a shoulder stand for eight minutes.

“I had a full life, creating art, working as a graphic designer, travelling overseas once a year. I had no limits. Now, my life is 30 per cent of that,” she said. It’s been 10 years since the fit ball burst.
Soula went to the doctor, was given pain medication and told to come back in eight weeks if the pain wasn’t reduced. Yet it worsened.
“Nerve pain, of course, doesn’t show on X-Rays,” she said. “It took me four and a half years to receive an accurate diagnosis. The pain would come and go with no routine. I would be fantastic one minute; the next I was spasming, burning, couldn’t function.”
Soula damaged the way her pudendal nerve, which stems from the sacrum and is responsible for motor supply to the pelvic muscles, signals the brain. When she sits, drives, lifts something, or moves suddenly, the nerve creates pain signals for no reason.
“I tried Lyrica (anti-siezure medication), nerve inhibitors, Tramadol (an opioid),” Soula said. She couldn’t work. She tried lying on her stomach on the studio floor, unable complete more than 15 minutes of work at one time.
“I took anti-depressants but these lowered my mood overall. My pain levels shifted constantly, and my GP told me to increase the dose of pain medication until it felt better.”
Soula became dependent. “I shrunk as a person. The medication fogged my mind. I couldn’t cross the road. I had to activate spell check on my phone. I didn’t have the ability to think properly any more,” she said.
“The most horrific part of this was the breathing. I would wake up in the middle of the night and realise I hadn’t taken a breath in ages. I would take a huge breath and start to panic.”









Hi Lisa. Firstly I hope you find some relief and wake up to a much better day today after your latest treatment. I’m sorry to hear about your battle with chronic pain – it’s absolutely grueling. The article is in no way intended for people who need to be on medication long-term. It’s aiming at reaching those unlike you, who don’t explore and persist exploring options. From my understanding the Alcohol & Drug Foundation are trying to discourage the ‘first stop’ recommendation for medication. I certainly would have liked that approach much better.
Hi, I have read many Posts. I had to write today. In the past I have found your site very helpful.
Today as I read, I’m in Hospital under the care of my Pain Management Dr. Who is a highly regarded Andthesist. I have been surviving Chronic Pain for over 12 years. My Purdendal nerve is compromised. Among other problems. I have tried two different nerve stimulation devices. For years each device. I have had stemcell treatment…..I have no choice but to continue Pain Management….. I hate having to take Pain relief, however without it my heart rate is so high from pain it compromises my life!!! I’m so happy for anyone who finds relief!!! Some of us have no choice but to take pain relief!