Where to next? (Part 2/3)
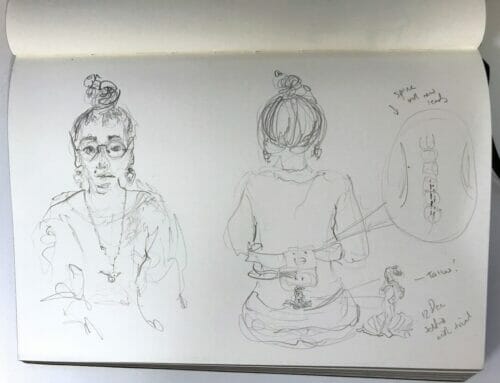
I knew there was something seriously wrong with my sacral stim implant.
By the time that information was confirmed, my mind had run off a few thousand questions. I’ll share a few:
Question number 1: What were my options for pain management now?
Firstly, I have to say, I didn’t feel alone facing this daunting process. Living with chronic pain can often leave you feeling alone, but I felt I had support and options – that’s really important.
My brilliant pain team keep me hopeful and resourced. I follow them online and I see all that they’re doing to keep up with the latest methods for pain management.
We were in constant communication and as soon as we figured out the sacral stim had to be removed, we began discussing options.
There were decisions to make, a trial to be had and I had to navigate this time with my peripheral stim which was working fine but not providing enough relief.
I learned alot in this time. I learned how much I have adapted life to manage chronic pain, how many sacrifices I make in the day, and how many Theo makes also.
With the commitment to move to a country town in order to find a way for me to work – self employment my only possibility, this meant I was far away from my best of friends and my family during a tough time.
I had to make plans to manage and care for myself and for Theo.
Theo works 7 days during summer – I can’t exactly hop on the bus. Theo working 7 days also meant he had much more than usual to manage in the day – he had to manage our lives even more than he does normally. Now there were also appointments in the mix which means complex, capacity swallowing, travel time.
The few chores I generally manage, I could no longer. I became slower and conversations, outings, tasks requiring focus were shrinking and becoming harder.
I looked the same. How do you explain this?
I’ve never made exercise a priority because my first aim was to use my capacity to get back to work (and remember, meds are not an option for me). This time, I made exercise a priority and sacrificed our social life and visitors.
I had to keep my walks up even though it impacted my capacity. My backpack was not full at the start of each day. I was running on low fuel.
Yes, not exercising causes pain but it still impacts capacity when you’re at the chronic level.
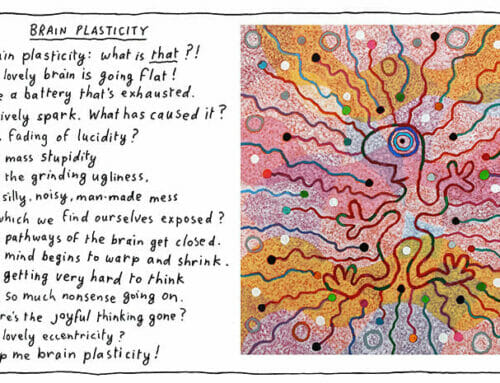
It’s hard to understand limited capacity that comes with chronic pain, and the varying levels and layers each of us endure and have to work through – impossible really.
I think the best way I can describe the limitations are by using the word fatigue and using a backpack as my prop (thanks PainRevolution)
Thoughts are tiring. Reading, talking, looking, seeing, thinking – it all, gets, tiring. Normal activity becomes even more tiring.
Looking, moving, shifting, shuffling, sitting, stepping aside, walking over, pointing… it all, gets, tiring. It all contributes to a brain shut down.
And the pain levels don’t necessarily go higher with more fatigue. So I can feel fatigued and have low pain levels. Or not feel fatigued and have screaming pain levels.
Who can possibly begin to understand what I’m saying? If you’ve read this far, you probably do.
Question number 2: Can I live with a Peripheral Stim?
I did consider staying with my peripheral stim to avoid more surgery. Why take more risks?
But as the weeks went on and my legs, feet, pain levels and fatigue started rising – all while I was reducing activity and becoming numb, I realised there wasn’t a choice.
And, NO! Meditating, natural therapies, exercise, and any other basic tips could not help.
NOTE: There’s chronic pain and there’s chronic pain. As much as we’d like to believe we can cure all, we can’t.
Only Theo can grasp the life change in those months. From the outside we both appeared normal, most people still believed I was working 7 days and had a great social life. No where on my social media is it possible to see that I live in a 1km radius most of the time.
I never post my down times.
If I didn’t want to work, I could venture further, use up more capacity and just rest before the next outing. But for me, the thought of resting just to socialising and never being creative is not an option.
Question number 3: Which Type of Stim?
It took some time to consider the options. Great to have a brilliant pain specialist who not only knows about all this, but Dr Christelis knows me and my situation. If you don’t feel this with your pain team, look elsewhere as this is super important.
Pain management is different for each of us. You need to be able to work that out with a specialist.
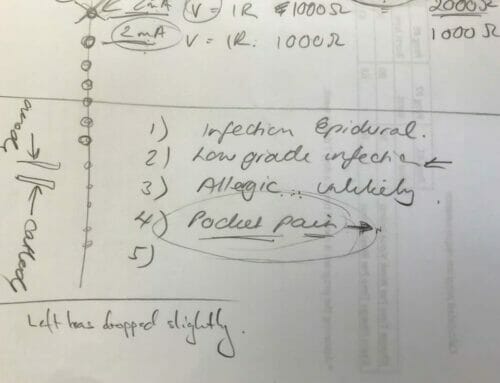
There were lots of questions, where to position leads and the battery, and of course which brand of stim.
I read up on the new stimwaves that don’t require an IPG. But the thought of wearing a belt all day, every day and every night would have me thinking about pain all day.
Last thing I felt I needed.
Did I want another Boston Scientific after what happened? Can I even be sure of what happened?!
I’m pretty sure the thing became very unwell and sadly getting to the bottom of the issue wasn’t worth it. It couldn’t be fixed. I needed to move on. I accepted, ‘We don’t know’.
I’ve endured 12 years of chronic pain, and by the time I’d be back on my feet again, I knew it would be another year.
Another year!
The only reason I decided against my original brand, St Judes (now renamed Abbott) and went for Boston Scientic is because it can provide four leads instead of two.
I’m assuming a new implant won’t die, again. And not that I’m presuming that my situation will worsen, but the option to add two more leads without a huge surgery, if necessary, is a much better long term plan.
Leads decided – they’re coming out of the sacrum and new ones are going into the spinal cord.
IPG decide – in my right bum cheek.
We set the date for the trial. I was ready months ago. This was all happening too late as far as I was concerned.
I contacted my WorkCover Agent and began preparing paperwork. I wasn’t going to wait for an insurer to approve my treatment. I was confident they wouldn’t give me trouble after my previous battles and victories with them.
Look out for the follow up report by the Ombudsman – released soon. I may be used as an example I’ve been told. Good!
And so, pretty much three years after my sacral stim was implanted, there I was again, back in hospital.
Question number 4: Will It work?
Impossible to know, but I expect so! But experiencing the past few months without my extra relief, I knew it was worth a trial and I could not live with just a peripheral stim. That would mean no more work – not even within my own special life setup.
I don’t want to live with the pain levels and without being able to work.
I’m, so, tired.








After 2 implants and removals over 8 years, I have given up on this for pudental and back pain. I feel for you. The never ending struggles and fatague from pain is a new Normal that I had to accept. I have traveled to other countries having to lay flat to do so. Life in increments etc …. Chronic Pain is a living nightmare. I can not work and my life is very isolated due to pain. I try my utmost for my family, but chronic pain has no “cure” it is now big business also! These stims companies are making huge money on the stock exchange! We are the guinea pigs.
I sincerely hope you find relief.
I can’t say my experience with the stims are bad, they give me great relief and quality of life so this glitch I hope will end up saving me another op down the track. It’s a really hard health issue but I don’t blame anyone, it’s the issue that is so horrible, not those who are trying to help us. They can only do their best and if you feel they’re not doing that for you, look elsewhere, even try the same treatment with another team. The team is everything. They are there when things go wrong just as much. I hope you find relief also. Life is short enough!
Soula,
I live in New Hampshire, USA. I think I may have some information that is helpful to you. I struggle with Pudendal Neuralgia but I am getting better with a physiotherapist.